Как правильно пишется слово «перинатальный»
перината́льный
Источник: Орфографический
академический ресурс «Академос» Института русского языка им. В.В. Виноградова РАН (словарная база
2020)
Делаем Карту слов лучше вместе
Привет! Меня зовут Лампобот, я компьютерная программа, которая помогает делать
Карту слов. Я отлично
умею считать, но пока плохо понимаю, как устроен ваш мир. Помоги мне разобраться!
Спасибо! Я стал чуточку лучше понимать мир эмоций.
Вопрос: инсайд — это что-то нейтральное, положительное или отрицательное?
Синонимы к слову «перинатальный»
Предложения со словом «перинатальный»
- Перинатальный период – это то время, когда закладывается сценарий человека, который потом отыгрывается на протяжении всей жизни в виде создания своего домашнего пространства.
- Перинатальный процесс тесно связан с биологическим рождением, но также включает в себя важные психологические, философские и духовные измерения.
- Неподалёку от дома находился перинатальный центр, и мама решила оформить меня туда.
- (все предложения)
Отправить комментарий
Смотрите также
-
Перинатальный период – это то время, когда закладывается сценарий человека, который потом отыгрывается на протяжении всей жизни в виде создания своего домашнего пространства.
-
Перинатальный процесс тесно связан с биологическим рождением, но также включает в себя важные психологические, философские и духовные измерения.
-
Неподалёку от дома находился перинатальный центр, и мама решила оформить меня туда.
- (все предложения)
- дополнительное обследование
- соматические заболевания
- апоплексия яичника
- объектные отношения
- вирусная нагрузка
- (ещё синонимы…)
перинатальный
- перинатальный
-
перинатальный
Слитно или раздельно? Орфографический словарь-справочник. — М.: Русский язык.
.
1998.
Синонимы:
Смотреть что такое «перинатальный» в других словарях:
-
ПЕРИНАТАЛЬНЫЙ — см. НАТАЛЬНЫЙ. Словарь иностранных слов. Комлев Н.Г., 2006. перинатальный (пери… + лат. natal is относящийся к рождению) относящийся к периоду непосредственно после родов (или к родам). Новый словарь иностранных слов. by EdwART, , 2009 … Словарь иностранных слов русского языка
-
перинатальный — прил., кол во синонимов: 1 • околородовой (1) Словарь синонимов ASIS. В.Н. Тришин. 2013 … Словарь синонимов
-
Перинатальный центр — Перинатальный медицинский центр это организация, в которой проводятся консультации, лечение и реабилитация беременных и родивших женщин, а также новорожденных, в т.ч. второй этап выхаживания, осуществляются ведение беременности и родов,… … Официальная терминология
-
ПЕРИНАТАЛЬНЫЙ ПЕРИОД — (от пери… и лат. natalis относящийся к рождению) охватывает внутриутробное развитие плода начиная с 28 недель беременности, период родов и первые 7 сут жизни ребенка … Большой Энциклопедический словарь
-
Перинатальный период — (от др. греч. peri около + лат. natalis относящийся к рождению) околородовой период; делится на: антенатальный (лат. ante перед) дородовой интранатальный (лат. intra внутри) непосредственно роды постнатальный (лат. post… … Википедия
-
Перинатальный период — начинается с 22 й полной недели (154 го дня) внутриутробной жизни плода (в это время в норме масса тела составляет 500 г) и заканчивается спустя 7 полных дней после рождения… Источник: ОХРАНА РЕПРОДУКТИВНОГО ЗДОРОВЬЯ РАБОТНИКОВ. ОСНОВНЫЕ… … Официальная терминология
-
перинатальный период — (от пери… и лат. natalis относящийся к рождению), охватывает внутриутробное развитие плода начиная с 28 недели беременности, период родов и первые 7 суток жизни ребёнка. * * * ПЕРИНАТАЛЬНЫЙ ПЕРИОД ПЕРИНАТАЛЬНЫЙ ПЕРИОД (от пери… (см. ПЕРИ…… … Энциклопедический словарь
-
перинатальный период — ЭМБРИОЛОГИЯ ЖИВОТНЫХ ПЕРИНАТАЛЬНЫЙ ПЕРИОД – у человека включает внутриутробное развитие плода за 10 суток до рождения и первые 7 суток после рождения … Общая эмбриология: Терминологический словарь
-
перинатальный — перинат альный … Русский орфографический словарь
-
перинатальный — … Орфографический словарь русского языка

Слова русского языка,
поиск и разбор слов онлайн
- Слова русского языка
- П
- перинатальный
Правильно слово пишется: перинатальный
Всего в слове 13 букв, 5 гласных, 7 согласных, 5 слогов.
Гласные: е, и, а, а, ы;
Согласные: п, р, н, т, л, н, й;
1 буква не обозначает звука.
Номера букв в слове
Номера букв в слове «перинатальный» в прямом и обратном порядке:
- 13
п
1 - 12
е
2 - 11
р
3 - 10
и
4 - 9
н
5 - 8
а
6 - 7
т
7 - 6
а
8 - 5
л
9 - 4
ь
10 - 3
н
11 - 2
ы
12 - 1
й
13
- Слова русского языка
- Русский язык
- О сайте
- Подборки слов
- Поиск слов по маске
- Составление словосочетаний
- Словосочетаний из предложений
- Деление слов на слоги
- Словари
- Орфографический словарь
- Словарь устаревших слов
- Словарь новых слов
- Орфография
- Орфограммы
- Проверка ошибок в словах
- Исправление ошибок
- Лексика
- Омонимы
- Устаревшие слова
- Заимствованные слова
- Новые слова
- Диалекты
- Слова-паразиты
- Сленговые слова
- Профессиональные слова
- Интересные слова
Рады помочь вам узнать, как пишется слово «перинатальный».
Пишите и говорите правильно.
О словаре
Сайт создан на основе «Русского орфографического словаря», составленного Институтом русского языка имени В. В. Виноградова РАН. Объем второго издания, исправленного и дополненного, составляет около 180 тысяч слов, и существенно превосходит все предшествующие орфографические словари. Он является нормативным справочником, отражающим с возможной полнотой лексику русского языка начала 21 века и регламентирующим ее правописание.
Как написать слово «перинатальный» правильно? Где поставить ударение, сколько в слове ударных и безударных гласных и согласных букв? Как проверить слово «перинатальный»?
перината́льный
Правильное написание — перинатальный, ударение падает на букву: а, безударными гласными являются: е, и, а, ы.
Выделим согласные буквы — перинатальный, к согласным относятся: п, р, н, т, л, й, звонкие согласные: р, н, л, й, глухие согласные: п, т.
Количество букв и слогов:
- букв — 13,
- слогов — 5,
- гласных — 5,
- согласных — 7.
Формы слова: перината́льный.
→
перинатальный — прилагательное, именительный п., муж. p., ед. ч.
↳
перинатальный — прилагательное, винительный п., муж. p., ед. ч.
Часть речи: прилагательное
Положительная степень:
| Единственное число | Множественное число | |||
|---|---|---|---|---|
| Мужской род | Женский род | Средний род | ||
| Им. |
перинатальный |
|||
| Рд. |
перинатального |
|||
| Дт. |
перинатальному |
|||
| Вн. |
перинатального перинатальный |
|||
| Тв. |
перинатальным |
|||
| Пр. |
перинатальном |
Если вы нашли ошибку, пожалуйста, выделите фрагмент текста и нажмите Ctrl+Enter.
|
|
См. также пренатальный. |
Содержание
- 1 Русский
- 1.1 Морфологические и синтаксические свойства
- 1.2 Произношение
- 1.3 Семантические свойства
- 1.3.1 Значение
- 1.3.2 Синонимы
- 1.3.3 Антонимы
- 1.3.4 Гиперонимы
- 1.3.5 Гипонимы
- 1.4 Родственные слова
- 1.5 Этимология
- 1.6 Фразеологизмы и устойчивые сочетания
- 1.7 Перевод
- 1.8 Библиография
Русский[править]
Морфологические и синтаксические свойства[править]
| падеж | ед. ч. | мн. ч. | |||
|---|---|---|---|---|---|
| муж. р. | ср. р. | жен. р. | |||
| Им. | перината́льный | перината́льное | перината́льная | перината́льные | |
| Р. | перината́льного | перината́льного | перината́льной | перината́льных | |
| Д. | перината́льному | перината́льному | перината́льной | перината́льным | |
| В. | одуш. | перината́льного | перината́льное | перината́льную | перината́льных |
| неод. | перината́льный | перината́льные | |||
| Т. | перината́льным | перината́льным | перината́льной перината́льною | перината́льными | |
| П. | перината́льном | перината́льном | перината́льной | перината́льных | |
| Кратк. форма | перината́лен | перината́льно | перината́льна | перината́льны |
пе—ри—на—та́ль—ный
Прилагательное, тип склонения по классификации А. Зализняка — 1*a.
Корень: —.
Произношение[править]
- МФА: [pʲɪrʲɪnɐˈtalʲnɨɪ̯]
Семантические свойства[править]
Значение[править]
- мед. относящийся к предродовому периоду, родам и первому времени после них ◆ Перинатальный период включает антенатальный (внутриутробное развитие плода), интранатальный (собственно роды) и постнатальный (ранний послеродовый период). Т. Ю. Соломатина, «Большая собака, или «Эклектичная живописная вавилонская повесть о зарытом»», 2009 г. [НКРЯ]
Синонимы[править]
- околородовой
Антонимы[править]
Гиперонимы[править]
Гипонимы[править]
Родственные слова[править]
| Ближайшее родство | |
|
Этимология[править]
Происходит от ??
Фразеологизмы и устойчивые сочетания[править]
- перинатальная йога
- перинатальный период
- перинатальная психология
- перинатальный сепсис
Перевод[править]
| Список переводов | |
|
Библиография[править]
- Новые слова и значения. Словарь-справочник по материалам прессы и литературы 80-х годов / Под ред. Е. А. Левашова. — СПб. : Дмитрий Буланин, 1997.
|
|
Для улучшения этой статьи желательно:
|
«Antenatal» redirects here. Not to be confused with Antinatalism.
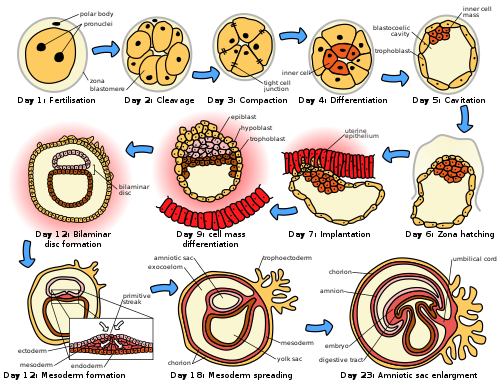
Prenatal development (from Latin natalis ‘relating to birth’) includes the development of the embryo and of the fetus during a viviparous animal’s gestation. Prenatal development starts with fertilization, in the germinal stage of embryonic development, and continues in fetal development until birth.
In human pregnancy, prenatal development is also called antenatal development. The development of the human embryo follows fertilization, and continues as fetal development. By the end of the tenth week of gestational age the embryo has acquired its basic form and is referred to as a fetus. The next period is that of fetal development where many organs become fully developed. This fetal period is described both topically (by organ) and chronologically (by time) with major occurrences being listed by gestational age.
The very early stages of embryonic development are the same in all mammals, but later stages of development, and the length of gestation varies.
Terminology[edit]
In the human:
Stages during pregnancy. Embryonic development is marked in green. Weeks and months are numbered by gestation.
Different terms are used to describe prenatal development, meaning development before birth. A term with the same meaning is the «antepartum» (from Latin ante «before» and parere «to give birth») Sometimes «antepartum» is however used to denote the period between the 24th/26th week of gestational age until birth, for example in antepartum hemorrhage.[1][2]
The perinatal period (from Greek peri, «about, around» and Latin nasci «to be born») is «around the time of birth». In developed countries and at facilities where expert neonatal care is available, it is considered from 22 completed weeks (usually about 154 days) of gestation (the time when birth weight is normally 500 g) to 7 completed days after birth.[3] In many of the developing countries the starting point of this period is considered 28 completed weeks of gestation (or weight more than 1000 g).[4]
Fertilization[edit]
Fertilization marks the first germinal stage of embryonic development. When semen is released into the vagina, the spermatozoa travel through the cervix, along the body of the uterus, and into one of the fallopian tubes where fertilization usually takes place in the ampulla. A great many sperm cells are released with the possibility of just one managing to adhere to and enter the thick protective layer surrounding the egg cell (ovum). The first sperm cell to successfully penetrate the egg cell donates its genetic material (DNA) to combine with the DNA of the egg cell resulting in a new one-celled zygote. The term «conception» refers variably to either fertilization or to formation of the conceptus after its implantation in the uterus, and this terminology is controversial.
The zygote will develop into a male if the egg is fertilized by a sperm that carries a Y chromosome, or a female if the sperm carries an X chromosome.[5] The Y chromosome contains a gene, SRY, which will switch on androgen production at a later stage leading to the development of a male body type. In contrast, the mitochondrial DNA of the zygote comes entirely from the egg cell.
Development of the embryo[edit]
Following fertilization, the embryonic stage of development continues until the end of the 10th week (gestational age) (8th week fertilization age). The first two weeks from fertilization is also referred to as the germinal stage or preembryonic stage.[6]
The zygote spends the next few days traveling down the fallopian tube dividing several times to form a ball of cells called a morula. Further cellular division is accompanied by the formation of a small cavity between the cells. This stage is called a blastocyst. Up to this point there is no growth in the overall size of the embryo, as it is confined within a glycoprotein shell, known as the zona pellucida. Instead, each division produces successively smaller cells.
The blastocyst reaches the uterus at roughly the fifth day after fertilization. The blastocyst hatches from the zona pellucida allowing the blastocyst’s outer cell layer of trophoblasts to come into contact with, and adhere to, the endometrial cells of the uterus. The trophoblasts will eventually give rise to extra-embryonic structures, such as the placenta and the membranes. The embryo becomes embedded in the endometrium in a process called implantation. In most successful pregnancies, the embryo implants 8 to 10 days after ovulation.[7] The embryo, the extra-embryonic membranes, and the placenta are collectively referred to as a conceptus, or the «products of conception».
Rapid growth occurs and the embryo’s main features begin to take form. This process is called differentiation, which produces the varied cell types (such as blood cells, kidney cells, and nerve cells). A spontaneous abortion, or miscarriage, in the first trimester of pregnancy is usually[8] due to major genetic mistakes or abnormalities in the developing embryo. During this critical period the developing embryo is also susceptible to toxic exposures, such as:
- Alcohol, certain drugs, and other toxins that cause birth defects, such as fetal alcohol syndrome
- Infection (such as rubella or cytomegalovirus)
- Radiation from x-rays or radiation therapy
- Nutritional deficiencies such as lack of folate which contributes to spina bifida
Nutrition[edit]
The embryo passes through 3 phases of acquisition of nutrition from the mother:[9]
- Absorption phase: Zygote is nourished by cellular cytoplasm and secretions in fallopian tubes and uterine cavity.[10]
- Histoplasmic transfer: After nidation and before establishment of uteroplacental circulation, embryonic nutrition is derived from decidual cells and maternal blood pools that open up as a result of eroding activity of trophoblasts.
- Hematotrophic phase: After third week of gestation, substances are transported passively via intervillous space.
Development of the fetus[edit]
The first ten weeks of gestational age is the period of embryogenesis and together with the first three weeks of prenatal development make up the first trimester of pregnancy.
From the 10th week of gestation (8th week of development), the developing embryo is called a fetus. All major structures are formed by this time, but they continue to grow and develop. Because the precursors of the organs are now formed, the fetus is not as sensitive to damage from environmental exposure as the embryo was. Instead, toxic exposure often causes physiological abnormalities or minor congenital malformation.
Development of organ systems[edit]
Development continues throughout the life of the fetus and through into life after birth. Significant changes occur to many systems in the period after birth as they adapt to life outside the uterus.
Fetal blood[edit]
Hematopoiesis first takes place in the yolk sac. The function is transferred to the liver by the 10th week of gestation and to the spleen and bone marrow beyond that. The total blood volume is about 125 ml/kg of fetal body weight near term.
Red blood cells[edit]
Megaloblastic red blood cells are produced early in development, which become normoblastic near term. Life span of prenatal RBCs is 80 days. Rh antigen appears at about 40 days of gestation.
White blood cells[edit]
The fetus starts producing leukocytes at 2 months gestational age, mainly from the thymus and the spleen. Lymphocytes derived from the thymus are called T lymphocytes (T cells), whereas those derived from bone marrow are called B lymphocytes (B cells). Both of these populations of lymphocytes have short-lived and long-lived groups. Short-lived T cells usually reside in thymus, bone marrow and spleen; whereas long-lived T cells reside in the blood stream. Plasma cells are derived from B cells and their life in fetal blood is 0.5 to 2 days.
Glands[edit]
The thyroid is the first gland to develop in the embryo at the 4th week of gestation. Insulin secretion in the fetus starts around the 12th week of gestation.
Cognitive development[edit]
Electrical brain activity is first detected at the end of week 5 of gestation, but as in brain-dead patients, it is primitive neural activity rather than the beginning of conscious brain activity. Synapses don’t begin to form until week 17.[11] Neural connections between the sensory cortex and thalamus develop as early as 24 weeks’ gestational age, but the first evidence of their function does not occur until around 30 weeks, when minimal consciousness, dreaming, and the ability to feel pain emerges.[12]
Initial knowledge of the effects of prenatal experience on later neuropsychological development originates from the Dutch Famine Study, which researched the cognitive development of individuals born after the Dutch famine of 1944–45.[13] The first studies focused on the consequences of the famine to cognitive development, including the prevalence of intellectual disability.[14] Such studies predate David Barker’s hypothesis about the association between the prenatal environment and the development of chronic conditions later in life.[15] The initial studies found no association between malnourishment and cognitive development,[14] but later studies found associations between malnourishment and increased risk for schizophrenia,[16] antisocial disorders,[17] and affective disorders.[18]
There is evidence that the acquisition of language begins in the prenatal stage. After 26 weeks of gestation, the peripheral auditory system is already fully formed.[19] Also, most low-frequency sounds (less than 300 Hz) can reach the fetal inner ear in the womb of mammals.[20] Those low-frequency sounds include pitch, rhythm, and phonetic information related to language.[21] Studies have indicated that fetuses react to and recognize differences between sounds.[22] Such ideas are further reinforced by the fact that newborns present a preference for their mother’s voice,[23] present behavioral recognition of stories only heard during gestation,[24] and (in monolingual mothers) present preference for their native language.[25] A more recent study with EEG demonstrated different brain activation in newborns hearing their native language compared to when they were presented with a different language, further supporting the idea that language learning starts while in gestation.[26]
Growth rate[edit]
The growth rate of a fetus is linear up to 37 weeks of gestation, after which it plateaus.[9] The growth rate of an embryo and infant can be reflected as the weight per gestational age, and is often given as the weight put in relation to what would be expected by the gestational age. A baby born within the normal range of weight for that gestational age is known as appropriate for gestational age (AGA). An abnormally slow growth rate results in the infant being small for gestational age, while an abnormally large growth rate results in the infant being large for gestational age. A slow growth rate and preterm birth are the two factors that can cause a low birth weight. Low birth weight (below 2000 grams) can slightly increase the likelihood of schizophrenia.[27]
The growth rate can be roughly correlated with the fundal height of the uterus which can be estimated by abdominal palpation. More exact measurements can be performed with obstetric ultrasonography.
Factors influencing development[edit]
Intrauterine growth restriction is one of the causes of low birth weight associated with over half of neonatal deaths.[28]
Poverty[edit]
Poverty has been linked to poor prenatal care and has been an influence on prenatal development. Women in poverty are more likely to have children at a younger age, which results in low birth weight. Many of these expecting mothers have little education and are therefore less aware of the risks of smoking, drinking alcohol, and drug use – other factors that influence the growth rate of a fetus.
Mother’s age[edit]
Women between the ages of 16 and 35 have a healthier environment for a fetus than women under 16 or over 35.[29] Women between this age gap are more likely to have fewer complications. Women over 35 are more inclined to have a longer labor period, which could potentially result in death of the mother or fetus. Women under 16 and over 35 have a higher risk of preterm labor (premature baby), and this risk increases for women in poverty, women who take drugs, and women who smoke. Young mothers are more likely to engage in high risk behaviors, such as using alcohol, drugs, or smoking, resulting in negative consequences for the fetus.[30] Premature babies from young mothers are more likely to have neurological defects that will influence their coping capabilities – irritability, trouble sleeping, constant crying for example. There is an increased risk of Down syndrome for infants born to those aged over 40 years. Young teenaged mothers (younger than 16) and mothers over 35 are more exposed to the risks of miscarriages, premature births, and birth defects.
Drug use[edit]
An estimated 5 percent of fetuses in the United States are exposed to illicit drug use during pregnancy.[31] Maternal drug use occurs when drugs ingested by the pregnant woman are metabolized in the placenta and then transmitted to the fetus. Recent research displays that there is a correlation between fine motor skills and prenatal risk factors such as the use of psychoactive substances and signs of abortion during pregnancy. As well as perinatal risk factors such as gestation time, duration of delivery, birth weight and postnatal risk factors such as constant falls.[32]
Cannabis[edit]
When using cannabis, there is a greater risk of birth defects, low birth weight, and a higher rate of death in infants or stillbirths.[33] Drug use will influence extreme irritability, crying, and risk for SIDS once the fetus is born.[34]
Marijuana will slow the fetal growth rate and can result in premature delivery. It can also lead to low birth weight, a shortened gestational period and complications in delivery.[33] Cannabis use during pregnancy was unrelated to risk of perinatal death or need for special care, but, the babies of women who used cannabis at least once per week before and throughout pregnancy were 216g lighter than those of non‐users, had significantly shorter birth lengths and smaller head circumferences.[35]
Opioids[edit]
Opioids including heroin will cause interrupted fetal development, stillbirths, and can lead to numerous birth defects. Heroin can also result in premature delivery, creates a higher risk of miscarriages, result in facial abnormalities and head size, and create gastrointestinal abnormalities in the fetus. There is an increased risk for SIDS, dysfunction in the central nervous system, and neurological dysfunctions including tremors, sleep problems, and seizures. The fetus is also put at a great risk for low birth weight and respiratory problems.[36]
Cocaine[edit]
Cocaine use results in a smaller brain, which results in learning disabilities for the fetus. Cocaine puts the fetus at a higher risk of being stillborn or premature. Cocaine use also results in low birthweight, damage to the central nervous system, and motor dysfunction. The vasoconstriction of the effects of cocaine lead to a decrease in placental blood flow to the fetus that results in fetal hypoxia (oxygen deficiency) and decreased fetal nutrition; these vasoconstrictive effects on the placenta have been linked to the number of complications in malformations that are evident in the newborn. [37]
Methamphetamine[edit]
Prenatal methamphetamine exposure has shown to negatively impact brain development and behavioral functioning. A 2019 study further investigated neurocognitive and neurodevelopmental effects of prenatal methamphetamine exposure. This study had two groups, one containing children who were prenatally exposed to methamphetamine but no other illicit drugs and one containing children who met diagnosis criteria for ADHD but were not prenatally exposed to any illicit substance. Both groups of children completed intelligence measures to compute an IQ. Study results showed that the prenatally exposed children performed lower on the intelligence measures than their non-exposed peers with ADHD. The study results also suggest that prenatal exposure to methamphetamine may negatively impact processing speed as children develop.[38]
Alcohol[edit]
Maternal alcohol use leads to disruptions of the fetus’s brain development, interferes with the fetus’s cell development and organization, and affects the maturation of the central nervous system. Even small amounts of alcohol use can cause lower height, weight and head size at birth and higher aggressiveness and lower intelligence during childhood.[39] Fetal alcohol spectrum disorder is a developmental disorder that is a consequence of heavy alcohol intake by the mother during pregnancy. Children with FASD have a variety of distinctive facial features, heart problems, and cognitive problems such as developmental disabilities, attention difficulties, and memory deficits.[39]
Tobacco use[edit]
Tobacco smoking during pregnancy exposes the fetus to nicotine, tar, and carbon monoxide. Nicotine results in less blood flow to the fetus because it constricts the blood vessels. Carbon monoxide reduces the oxygen flow to the fetus. The reduction of blood and oxygen flow may result in miscarriage, stillbirth, low birth weight, and premature births.[40] Exposure to secondhand smoke leads to higher risks of low birth weight and childhood cancer.[41]
Infections[edit]
If a mother is infected with a disease, the placenta cannot always filter out the pathogens. Viruses such as rubella, chicken pox, mumps, herpes, and human immunodeficiency virus (HIV) are associated with an increased risk of miscarriage, low birth weight, prematurity, physical malformations, and intellectual disabilities.[42] HIV can lead to acquired immune deficiency syndrome (AIDS). Untreated HIV carries a risk of between 10 and 20 per cent of being passed on to the fetus.[43] Bacterial or parasitic diseases may also be passed on to the fetus, and include chlamydia, syphilis, tuberculosis, malaria, and commonly toxoplasmosis.[44] Toxoplasmosis can be acquired through eating infected undercooked meat or contaminated food, and by drinking contaminated water.[45] The risk of fetal infection is lowest during early pregnancy, and highest during the third trimester. However, in early pregnancy the outcome is worse, and can be fatal.[45]
Maternal nutrition[edit]
Adequate nutrition is needed for a healthy fetus. Mothers who gain less than 20 pounds during pregnancy are at increased risk for having a preterm or low birth weight infant.[46] Iron and iodine are especially important during prenatal development. Mothers who are deficient in iron are at risk for having a preterm or low birth weight infant.[47] Iodine deficiencies increase the risk of miscarriage, stillbirth, and fetal brain abnormalities. Adequate prenatal care gives an improved result in the newborn.[48]
Low birth weight[edit]
Low birth weight increases an infants risk of long-term growth and cognitive and language deficits. It also results in a shortened gestational period and can lead to prenatal complications.
Stress[edit]
Stress during pregnancy can have an impact the development of the embryo. Reilly (2017) states that stress can come from many forms of life events such as community, family, financial issues, and natural causes. While a woman is pregnant, stress from outside sources can take a toll on the growth in the womb that may affect the child’s learning and relationships when born. For instance, they may have behavioral problems and might be antisocial. The stress that the mother experiences affects the fetus and the fetus’ growth which can include the fetus’ nervous system (Reilly, 2017). Stress can also lead to low birth weight. Even after avoiding other factors like alcohol, drugs, and being healthy, stress can have its impacts whether families know it or not. Many women who deal with maternal stress do not seek treatment.
Similar to stress, Reilly stated that in recent studies, researchers have found that pregnant women who show depressive symptoms are not as attached and bonded to their child while it is in the womb (2017).[49]
Environmental toxins[edit]
Exposure to environmental toxins in pregnancy lead to higher rates of miscarriage, sterility, and birth defects. Toxins include fetal exposure to lead, mercury, and ethanol or hazardous environments. Prenatal exposure to mercury may lead to physical deformation, difficulty in chewing and swallowing, and poor motoric coordination.[50] Exposure to high levels of lead prenatally is related to prematurity, low birth weight, brain damage, and a variety of physical defects.[50] Exposure to persistent air pollution from traffic and smog may lead to reduced infant head size, low birth weight, increased infant death rates, impaired lung and immune system development.[51]
See also[edit]
- Prenatal memory
- Prenatal and perinatal psychology
- Fetal pig
- Timeline of human prenatal development
- Transplacental carcinogenesis
References[edit]
- ^ patient.info » PatientPlus » Antepartum Haemorrhage Last Updated: 5 May 2009
- ^ The Royal Women’s Hospital > antepartum haemorrhage Archived 8 January 2010 at the Wayback Machine Retrieved on 13 Jan 2009
- ^ Definitions and Indicators in Family Planning. Maternal & Child Health and Reproductive Health. Archived 25 January 2012 at the Wayback Machine By European Regional Office, World Health Organization. Revised March 1999 & January 2001. In turn citing: WHO Geneva, WHA20.19, WHA43.27, Article 23
- ^ Singh, Meharban (2010). Care of the Newborn. p. 7. Edition 7. ISBN 9788170820536
- ^ Schacter, Daniel (2009). «11-Development». Psychology Second Edition. United States of America: Worth Publishers. ISBN 978-1-4292-3719-2.
- ^ Saladin, Kenneth (2011). Human anatomy (3rd ed.). McGraw-Hill. p. 85. ISBN 9780071222075.
- ^ Wilcox AJ, Baird DD, Weinberg CR (1999). «Time of implantation of the conceptus and loss of pregnancy». N. Engl. J. Med. 340 (23): 1796–9. doi:10.1056/NEJM199906103402304. PMID 10362823.
- ^ Moore L. Keith. (2008). Before We Are Born: Essentials of Embryology and Birth Defects. Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-3705-7.
- ^ a b Daftary, Shirish; Chakravarti, Sudip (2011). Manual of Obstetrics, 3rd Edition. Elsevier. pp. 1–16. ISBN 9788131225561.
- ^ «Fetal development: MedlinePlus Medical Encyclopedia». medlineplus.gov. Retrieved 7 April 2021.
- ^ Illes J, ed. (2008). Neuroethics : defining the issues in theory, practice, and policy (Repr. ed.). Oxford: Oxford University Press. p. 142. ISBN 978-0-19-856721-9. Archived from the original on 19 September 2015.
- ^
- Harley, Trevor A. (2021). The Science of Consciousness: Waking, Sleeping and Dreaming. Cambridge, United Kingdom: Cambridge University Press. p. 245. ISBN 978-1-107-12528-5. Retrieved 3 May 2022.
- Cleeremans, Axel; Wilken, Patrick; Bayne, Tim, eds. (2009). The Oxford Companion to Consciousness. New York, NY: Oxford University Press. p. 229. ISBN 978-0-19-856951-0. Retrieved 3 May 2022.
- Thompson, Evan; Moscovitch, Morris; Zelazo, Philip David, eds. (2007). The Cambridge Handbook of Consciousness. Cambridge, United Kingdom: Cambridge University Press. pp. 415–417. ISBN 9781139464062. Retrieved 3 May 2022.
- ^ Henrichs, J. (2010). Prenatal determinants of early behavioral and cognitive development: The generation R study. Rotteram: Erasmus Universiteit.
- ^ a b Stein, Z., Susser, M., Saenger, G., & Marolla, F. (1972). Nutrition and mental performance. Science, 178(62),708-713.
- ^ Barker, D. J., Winter, P. D., Osmond, C., Margetts, B., & Simmonds, S. J. (1989). Weight in infancy and death from ischaemic heart disease. Lancet, 2(8663), 577-580.
- ^ Brown, A.S.; Susser, E.S.; Hoek, H.W.; Neugebauer, R.; Lin, S.P.; Gorman, J.M. (1996). «Schizophrenia and affective disorders after prenatal famine». Biological Psychiatry. 39 (7): 551. doi:10.1016/0006-3223(96)84122-9. S2CID 54389015.
- ^ Neugebauer, R., Hoek, H. W., & Susser, E. (1999). Prenatal exposure to wartime famine and development of antisocial personality disorder in early adulthood. Jama, 282(5), 455-462.
- ^ Brown, A. S., van Os, J., Driessens, C., Hoek, H. W., & Susser, E. S. (2000). Further evidence of relation between prenatal famine and major affective disorder. American Journal of Psychiatry, 157(2), 190-195.
- ^ Eisenberg, R. B. (1976). Auditory Competence in Early Life: The Roots of Communicate Behavior Baltimore: University Park Press.
- ^ Gerhardt, K. J., Otto, R., Abrams, R. M., Colle, J. J., Burchfield, D. J., and Peters, A. J. M. (1992). Cochlear microphones recorded from fetal and newborn sheep. Am. J. Otolaryngol. 13, 226–233.
- ^ Lecaneut, J. P., and Granier-Deferre, C. (1993). «Speech stimuli in the fetal environment», in Developmental Neurocognition: Speech and Face Processing in the First Year of Life, eds B. De Boysson-Bardies, S. de Schonen, P. Jusczyk, P. MacNeilage, and J. Morton (Norwell, MA: Kluwer Academic Publishing), 237–248.
- ^ Kisilevsky, B. S., Hains, S. M. J., Lee, K., Xie, X., Ye, H. H., Zhang, K., and Wang, Z. (2003). Effects of experience on fetal voice recognition. Psychol. Sci. 14, 220–224.
- ^ DeCasper, A. J., and Fifer, W. P. (1980). Of human bonding: newborns prefer their mother’s voices. Science 208, 1174–1176.
- ^ DeCasper, A. J., and Spence, M. J. (1986). Prenatal maternal speech influences newborns’ perception of speech sounds. Infant Behav. Dev. 9, 133–150.
- ^ Moon, C., Cooper, R. P., and Fifer, W. P. (1993). Two-day-olds prefer their native language. Infant Behav. Dev. 16, 495–500.
- ^ May, Lillian; Byers-Heinlein, Krista; Gervain, Judit; Werker, Janet F. (2011). «Language and the Newborn Brain: Does Prenatal Language Experience Shape the Neonate Neural Response to Speech?». Frontiers in Psychology. 2: 222. doi:10.3389/fpsyg.2011.00222. PMC 3177294. PMID 21960980.
- ^ King, Suzanne; St-Hilaire, Annie; Heidkamp, David (2010). «Prenatal Factors in Schizophrenia». Current Directions in Psychological Science. 19 (4): 209–213. doi:10.1177/0963721410378360. S2CID 145368617.
- ^ Lawn JE, Cousens S, Zupan J (2005). «4 million neonatal deaths: when? Where? Why?». The Lancet. 365 (9462): 891–900. doi:10.1016/s0140-6736(05)71048-5. PMID 15752534. S2CID 20891663.
- ^ Centers for Disease Control (2018). «Pregnancy Complications». Centers for Disease Control.
- ^ «About Teenage Pregnancy». Centers for Disease Control. 2018. Archived from the original on 2018.
- ^ Wendell, A. D. (2013). «Overview and epidemiology of substance abuse in pregnancy». Clinical Obstetrics & Gynecology. 56 (1): 91–96. doi:10.1097/GRF.0b013e31827feeb9. PMID 23314721. S2CID 44402625.
- ^ Lerma Castaño, Piedad Rocio; Montealegre Suarez, Diana Paola; Mantilla Toloza, Sonia Carolina; Jaimes Guerrero, Carlos Alberto; Romaña Cabrera, Luisa Fernanda; Lozano Mañosca, Daiana Stefanny (2021). «Prenatal, perinatal and postnatal risk factors associated with fine motor function delay in pre-school children in Neiva, Colombia». Early Child Development and Care. 191 (16): 2600–2606. doi:10.1080/03004430.2020.1726903. S2CID 216219379.
- ^ a b Fonseca, B. M.; Correia-da-Silva, G.; Almada, M.; Costa, M. A.; Teixeira, N. A. (2013). «The Endocannabinoid System in the Postimplantation Period: A Role during Decidualization and Placentation». International Journal of Endocrinology. 2013: 510540. doi:10.1155/2013/510540. PMC 3818851. PMID 24228028.
- ^ Irner, Tina Birk (November 2012). «Substance exposure in utero and developmental consequences in adolescence: A systematic review». Child Neuropsychology. 18 (6): 521–549. doi:10.1080/09297049.2011.628309. PMID 22114955. S2CID 25014303.
- ^ Fergusson, David M.; Horwood, L. John; Northstone, Kate (2002). «Maternal use of cannabis and pregnancy outcome». BJOG: An International Journal of Obstetrics & Gynaecology. 109 (1): 21–27. doi:10.1111/j.1471-0528.2002.01020.x. ISSN 1471-0528. PMID 11843371. S2CID 22461729.
- ^ «The US Opioid Crisis: Addressing Maternal and Infant Health». Centers of Disease Control and Prevention. 29 May 2019.
- ^ Mayes, Linda C. (1992). «Prenatal Cocaine Exposure and Young Children’s Development». The Annals of the American Academy of Political and Social Science. 521: 11–27. doi:10.1177/0002716292521001002. JSTOR 1046540. S2CID 72963424.
- ^ Brinker, Michael J.; Cohen, Jodie G.; Sharrette, Johnathan A.; Hall, Trevor A. (2019). «Neurocognitive and neurodevelopmental impact of prenatal methamphetamine exposure: A comparison study of prenatally exposed children with nonexposed ADHD peers». Applied Neuropsychology: Child. 8 (2): 132–139. doi:10.1080/21622965.2017.1401479. PMID 29185821. S2CID 25747787.
- ^ a b Mattson, Sarah N.; Roesch, Scott C.; Fagerlund, Åse; Autti-Rämö, Ilona; Jones, Kenneth Lyons; May, Philip A.; Adnams, Colleen M.; Konovalova, Valentina; Riley, Edward P. (21 June 2010). «Toward a Neurobehavioral Profile of Fetal Alcohol Spectrum Disorders». Alcoholism: Clinical and Experimental Research. 34 (9): 1640–1650. doi:10.1111/j.1530-0277.2010.01250.x. ISSN 0145-6008. PMC 2946199. PMID 20569243.
- ^ Espy, Kimberly Andrews; Fang, Hua; Johnson, Craig; Stopp, Christian; Wiebe, Sandra A.; Respass, Jennifer (2011). «Prenatal tobacco exposure: Developmental outcomes in the neonatal period». Developmental Psychology. 47 (1): 153–169. doi:10.1037/a0020724. ISSN 1939-0599. PMC 3057676. PMID 21038943.
- ^ Rückinger, Simon; Beyerlein, Andreas; Jacobsen, Geir; von Kries, Rüdiger; Vik, Torstein (December 2010). «Growth in utero and body mass index at age 5years in children of smoking and non-smoking mothers». Early Human Development. 86 (12): 773–777. doi:10.1016/j.earlhumdev.2010.08.027. ISSN 0378-3782. PMID 20869819.
- ^ Waldorf, K. M. A. (2013). «Influence of infection during pregnancy on fetal development». Reproduction. 146 (5): 151–162. doi:10.1530/REP-13-0232. PMC 4060827. PMID 23884862.
- ^ «World health statistics». World Health Organization. 2014.
- ^ Diav-Citrin, O (2011). «Prenatal exposures associated with neurodevelopmental delay and disabilities». Developmental Disabilities Research Reviews. 17 (2): 71–84. doi:10.1002/ddrr.1102. PMID 23362027.
- ^ a b Bobić, B; Villena, I; Stillwaggon, E (September 2019). «Prevention and mitigation of congenital toxoplasmosis. Economic costs and benefits in diverse settings». Food and Waterborne Parasitology (Online). 16: e00058. doi:10.1016/j.fawpar.2019.e00058. PMC 7034037. PMID 32095628.
- ^ Ehrenberg, H (2003). «Low maternal weight, failure to thrive in pregnancy, and adverse pregnancy outcomes». American Journal of Obstetrics and Gynecology. 189 (6): 1726–1730. doi:10.1016/S0002-9378(03)00860-3. PMID 14710105.
- ^ «Micronutrient deficiencies». World Health Organization. 2002. Archived from the original on 5 December 1998.
- ^ «What is prenatal care and why is it important?». www.nichd.nih.gov.
- ^ Reilly, Nicole (2017). «Stress, depression and anxiety during pregnancy: How does it impact on children and how can we intervene early?». International Journal of Birth & Parent Education. 5 (1): 9–12.
- ^ a b Caserta, D (2013). «Heavy metals and placental fetal-maternal barrier: A mini review on the major concerns». European Review for Medical and Pharmacological Sciences. 17 (16): 2198–2206. PMID 23893187.
- ^ Proietti, E (2013). «Air pollution during pregnancy and neonatal outcome: A review». Journal of Aerosol Medicine and Pulmonary Drug Delivery. 26 (1): 9–23. doi:10.1089/jamp.2011.0932. PMID 22856675.
Further reading[edit]
- MedlinePlus Encyclopedia: Fetal development
- Moore, Keith L. (1998). The Developing Human (3rd ed.). Philadelphia PA: W.B. Saunders Company. ISBN 9780721669748.
- Wilcox AJ, Baird DD, Weinberg CR (June 1999). «Time of implantation of the conceptus and loss of pregnancy». N. Engl. J. Med. 340 (23): 1796–9. doi:10.1056/NEJM199906103402304. PMID 10362823.
- Ljunger E, Cnattingius S, Lundin C, Annerén G (November 2005). «Chromosomal anomalies in first-trimester miscarriages». Acta Obstet Gynecol Scand. 84 (11): 1103–7. doi:10.1111/j.0001-6349.2005.00882.x. PMID 16232180. S2CID 40039636.
- Newman, Barbara; Newman, Philip (10 March 2008). «The Period of Pregnancy and Prenatal Development». Development Through Life: A Psychosocial Approach. Cengage Learning. ISBN 978-0-495-55341-0.
- «Prenatal Development – Prenatal Environmental Influences – Mother, Birth, Fetus, and Pregnancy.» Social Issues Reference. Version Child Development Vol. 6. N.p., n.d. Web. 19 Nov. 2012.
- Niedziocha, Laura. «The Effects of Drugs And Alcohol on Fetal Development | LIVESTRONG.COM.» LIVESTRONG.COM – Lose Weight & Get Fit with Diet, Nutrition & Fitness Tools | LIVESTRONG.COM. N.p., 4 Sept. 2011. Web. 19 Nov. 2012. <http://www.livestrong.com/article/535499-the-effects-of-drugs-and-alcohol-on-fetal-development/>.
- Jaakkola, JJ; Gissler, M (January 2004). «Maternal smoking in pregnancy, fetal development, and childhood asthma». American Journal of Public Health. 94 (1): 136–40. doi:10.2105/ajph.94.1.136. PMC 1449839. PMID 14713711.
- Gutbrod, T (1 May 2000). «Effects of gestation and birth weight on the growth and development of very low birthweight small for gestational age infants: a matched group comparison». Archives of Disease in Childhood: Fetal and Neonatal Edition. 82 (3): 208F–214. doi:10.1136/fn.82.3.F208. PMC 1721075. PMID 10794788.
- Brady, Joanne P., Marc Posner, and Cynthia Lang. «Risk and Reality: The Implications of Prenatal Exposure to Alcohol and Other Drugs .» ASPE. N.p., n.d. Web. 19 Nov. 2012. <http://aspe.hhs.gov/hsp/cyp/drugkids.htm>.
External links[edit]
Wikimedia Commons has media related to Embryology.
- Chart of human fetal development, U.S. National Library of Medicine (NLM)
- U.K. Human Fertilisation and Embryology Authority (HFEA), regulatory agency overseeing the use of gametes and embryos in fertility treatment and research
«Antenatal» redirects here. Not to be confused with Antinatalism.
Prenatal development (from Latin natalis ‘relating to birth’) includes the development of the embryo and of the fetus during a viviparous animal’s gestation. Prenatal development starts with fertilization, in the germinal stage of embryonic development, and continues in fetal development until birth.
In human pregnancy, prenatal development is also called antenatal development. The development of the human embryo follows fertilization, and continues as fetal development. By the end of the tenth week of gestational age the embryo has acquired its basic form and is referred to as a fetus. The next period is that of fetal development where many organs become fully developed. This fetal period is described both topically (by organ) and chronologically (by time) with major occurrences being listed by gestational age.
The very early stages of embryonic development are the same in all mammals, but later stages of development, and the length of gestation varies.
Terminology[edit]
In the human:
Stages during pregnancy. Embryonic development is marked in green. Weeks and months are numbered by gestation.
Different terms are used to describe prenatal development, meaning development before birth. A term with the same meaning is the «antepartum» (from Latin ante «before» and parere «to give birth») Sometimes «antepartum» is however used to denote the period between the 24th/26th week of gestational age until birth, for example in antepartum hemorrhage.[1][2]
The perinatal period (from Greek peri, «about, around» and Latin nasci «to be born») is «around the time of birth». In developed countries and at facilities where expert neonatal care is available, it is considered from 22 completed weeks (usually about 154 days) of gestation (the time when birth weight is normally 500 g) to 7 completed days after birth.[3] In many of the developing countries the starting point of this period is considered 28 completed weeks of gestation (or weight more than 1000 g).[4]
Fertilization[edit]
Fertilization marks the first germinal stage of embryonic development. When semen is released into the vagina, the spermatozoa travel through the cervix, along the body of the uterus, and into one of the fallopian tubes where fertilization usually takes place in the ampulla. A great many sperm cells are released with the possibility of just one managing to adhere to and enter the thick protective layer surrounding the egg cell (ovum). The first sperm cell to successfully penetrate the egg cell donates its genetic material (DNA) to combine with the DNA of the egg cell resulting in a new one-celled zygote. The term «conception» refers variably to either fertilization or to formation of the conceptus after its implantation in the uterus, and this terminology is controversial.
The zygote will develop into a male if the egg is fertilized by a sperm that carries a Y chromosome, or a female if the sperm carries an X chromosome.[5] The Y chromosome contains a gene, SRY, which will switch on androgen production at a later stage leading to the development of a male body type. In contrast, the mitochondrial DNA of the zygote comes entirely from the egg cell.
Development of the embryo[edit]
Following fertilization, the embryonic stage of development continues until the end of the 10th week (gestational age) (8th week fertilization age). The first two weeks from fertilization is also referred to as the germinal stage or preembryonic stage.[6]
The zygote spends the next few days traveling down the fallopian tube dividing several times to form a ball of cells called a morula. Further cellular division is accompanied by the formation of a small cavity between the cells. This stage is called a blastocyst. Up to this point there is no growth in the overall size of the embryo, as it is confined within a glycoprotein shell, known as the zona pellucida. Instead, each division produces successively smaller cells.
The blastocyst reaches the uterus at roughly the fifth day after fertilization. The blastocyst hatches from the zona pellucida allowing the blastocyst’s outer cell layer of trophoblasts to come into contact with, and adhere to, the endometrial cells of the uterus. The trophoblasts will eventually give rise to extra-embryonic structures, such as the placenta and the membranes. The embryo becomes embedded in the endometrium in a process called implantation. In most successful pregnancies, the embryo implants 8 to 10 days after ovulation.[7] The embryo, the extra-embryonic membranes, and the placenta are collectively referred to as a conceptus, or the «products of conception».
Rapid growth occurs and the embryo’s main features begin to take form. This process is called differentiation, which produces the varied cell types (such as blood cells, kidney cells, and nerve cells). A spontaneous abortion, or miscarriage, in the first trimester of pregnancy is usually[8] due to major genetic mistakes or abnormalities in the developing embryo. During this critical period the developing embryo is also susceptible to toxic exposures, such as:
- Alcohol, certain drugs, and other toxins that cause birth defects, such as fetal alcohol syndrome
- Infection (such as rubella or cytomegalovirus)
- Radiation from x-rays or radiation therapy
- Nutritional deficiencies such as lack of folate which contributes to spina bifida
Nutrition[edit]
The embryo passes through 3 phases of acquisition of nutrition from the mother:[9]
- Absorption phase: Zygote is nourished by cellular cytoplasm and secretions in fallopian tubes and uterine cavity.[10]
- Histoplasmic transfer: After nidation and before establishment of uteroplacental circulation, embryonic nutrition is derived from decidual cells and maternal blood pools that open up as a result of eroding activity of trophoblasts.
- Hematotrophic phase: After third week of gestation, substances are transported passively via intervillous space.
Development of the fetus[edit]
The first ten weeks of gestational age is the period of embryogenesis and together with the first three weeks of prenatal development make up the first trimester of pregnancy.
From the 10th week of gestation (8th week of development), the developing embryo is called a fetus. All major structures are formed by this time, but they continue to grow and develop. Because the precursors of the organs are now formed, the fetus is not as sensitive to damage from environmental exposure as the embryo was. Instead, toxic exposure often causes physiological abnormalities or minor congenital malformation.
Development of organ systems[edit]
Development continues throughout the life of the fetus and through into life after birth. Significant changes occur to many systems in the period after birth as they adapt to life outside the uterus.
Fetal blood[edit]
Hematopoiesis first takes place in the yolk sac. The function is transferred to the liver by the 10th week of gestation and to the spleen and bone marrow beyond that. The total blood volume is about 125 ml/kg of fetal body weight near term.
Red blood cells[edit]
Megaloblastic red blood cells are produced early in development, which become normoblastic near term. Life span of prenatal RBCs is 80 days. Rh antigen appears at about 40 days of gestation.
White blood cells[edit]
The fetus starts producing leukocytes at 2 months gestational age, mainly from the thymus and the spleen. Lymphocytes derived from the thymus are called T lymphocytes (T cells), whereas those derived from bone marrow are called B lymphocytes (B cells). Both of these populations of lymphocytes have short-lived and long-lived groups. Short-lived T cells usually reside in thymus, bone marrow and spleen; whereas long-lived T cells reside in the blood stream. Plasma cells are derived from B cells and their life in fetal blood is 0.5 to 2 days.
Glands[edit]
The thyroid is the first gland to develop in the embryo at the 4th week of gestation. Insulin secretion in the fetus starts around the 12th week of gestation.
Cognitive development[edit]
Electrical brain activity is first detected at the end of week 5 of gestation, but as in brain-dead patients, it is primitive neural activity rather than the beginning of conscious brain activity. Synapses don’t begin to form until week 17.[11] Neural connections between the sensory cortex and thalamus develop as early as 24 weeks’ gestational age, but the first evidence of their function does not occur until around 30 weeks, when minimal consciousness, dreaming, and the ability to feel pain emerges.[12]
Initial knowledge of the effects of prenatal experience on later neuropsychological development originates from the Dutch Famine Study, which researched the cognitive development of individuals born after the Dutch famine of 1944–45.[13] The first studies focused on the consequences of the famine to cognitive development, including the prevalence of intellectual disability.[14] Such studies predate David Barker’s hypothesis about the association between the prenatal environment and the development of chronic conditions later in life.[15] The initial studies found no association between malnourishment and cognitive development,[14] but later studies found associations between malnourishment and increased risk for schizophrenia,[16] antisocial disorders,[17] and affective disorders.[18]
There is evidence that the acquisition of language begins in the prenatal stage. After 26 weeks of gestation, the peripheral auditory system is already fully formed.[19] Also, most low-frequency sounds (less than 300 Hz) can reach the fetal inner ear in the womb of mammals.[20] Those low-frequency sounds include pitch, rhythm, and phonetic information related to language.[21] Studies have indicated that fetuses react to and recognize differences between sounds.[22] Such ideas are further reinforced by the fact that newborns present a preference for their mother’s voice,[23] present behavioral recognition of stories only heard during gestation,[24] and (in monolingual mothers) present preference for their native language.[25] A more recent study with EEG demonstrated different brain activation in newborns hearing their native language compared to when they were presented with a different language, further supporting the idea that language learning starts while in gestation.[26]
Growth rate[edit]
The growth rate of a fetus is linear up to 37 weeks of gestation, after which it plateaus.[9] The growth rate of an embryo and infant can be reflected as the weight per gestational age, and is often given as the weight put in relation to what would be expected by the gestational age. A baby born within the normal range of weight for that gestational age is known as appropriate for gestational age (AGA). An abnormally slow growth rate results in the infant being small for gestational age, while an abnormally large growth rate results in the infant being large for gestational age. A slow growth rate and preterm birth are the two factors that can cause a low birth weight. Low birth weight (below 2000 grams) can slightly increase the likelihood of schizophrenia.[27]
The growth rate can be roughly correlated with the fundal height of the uterus which can be estimated by abdominal palpation. More exact measurements can be performed with obstetric ultrasonography.
Factors influencing development[edit]
Intrauterine growth restriction is one of the causes of low birth weight associated with over half of neonatal deaths.[28]
Poverty[edit]
Poverty has been linked to poor prenatal care and has been an influence on prenatal development. Women in poverty are more likely to have children at a younger age, which results in low birth weight. Many of these expecting mothers have little education and are therefore less aware of the risks of smoking, drinking alcohol, and drug use – other factors that influence the growth rate of a fetus.
Mother’s age[edit]
Women between the ages of 16 and 35 have a healthier environment for a fetus than women under 16 or over 35.[29] Women between this age gap are more likely to have fewer complications. Women over 35 are more inclined to have a longer labor period, which could potentially result in death of the mother or fetus. Women under 16 and over 35 have a higher risk of preterm labor (premature baby), and this risk increases for women in poverty, women who take drugs, and women who smoke. Young mothers are more likely to engage in high risk behaviors, such as using alcohol, drugs, or smoking, resulting in negative consequences for the fetus.[30] Premature babies from young mothers are more likely to have neurological defects that will influence their coping capabilities – irritability, trouble sleeping, constant crying for example. There is an increased risk of Down syndrome for infants born to those aged over 40 years. Young teenaged mothers (younger than 16) and mothers over 35 are more exposed to the risks of miscarriages, premature births, and birth defects.
Drug use[edit]
An estimated 5 percent of fetuses in the United States are exposed to illicit drug use during pregnancy.[31] Maternal drug use occurs when drugs ingested by the pregnant woman are metabolized in the placenta and then transmitted to the fetus. Recent research displays that there is a correlation between fine motor skills and prenatal risk factors such as the use of psychoactive substances and signs of abortion during pregnancy. As well as perinatal risk factors such as gestation time, duration of delivery, birth weight and postnatal risk factors such as constant falls.[32]
Cannabis[edit]
When using cannabis, there is a greater risk of birth defects, low birth weight, and a higher rate of death in infants or stillbirths.[33] Drug use will influence extreme irritability, crying, and risk for SIDS once the fetus is born.[34]
Marijuana will slow the fetal growth rate and can result in premature delivery. It can also lead to low birth weight, a shortened gestational period and complications in delivery.[33] Cannabis use during pregnancy was unrelated to risk of perinatal death or need for special care, but, the babies of women who used cannabis at least once per week before and throughout pregnancy were 216g lighter than those of non‐users, had significantly shorter birth lengths and smaller head circumferences.[35]
Opioids[edit]
Opioids including heroin will cause interrupted fetal development, stillbirths, and can lead to numerous birth defects. Heroin can also result in premature delivery, creates a higher risk of miscarriages, result in facial abnormalities and head size, and create gastrointestinal abnormalities in the fetus. There is an increased risk for SIDS, dysfunction in the central nervous system, and neurological dysfunctions including tremors, sleep problems, and seizures. The fetus is also put at a great risk for low birth weight and respiratory problems.[36]
Cocaine[edit]
Cocaine use results in a smaller brain, which results in learning disabilities for the fetus. Cocaine puts the fetus at a higher risk of being stillborn or premature. Cocaine use also results in low birthweight, damage to the central nervous system, and motor dysfunction. The vasoconstriction of the effects of cocaine lead to a decrease in placental blood flow to the fetus that results in fetal hypoxia (oxygen deficiency) and decreased fetal nutrition; these vasoconstrictive effects on the placenta have been linked to the number of complications in malformations that are evident in the newborn. [37]
Methamphetamine[edit]
Prenatal methamphetamine exposure has shown to negatively impact brain development and behavioral functioning. A 2019 study further investigated neurocognitive and neurodevelopmental effects of prenatal methamphetamine exposure. This study had two groups, one containing children who were prenatally exposed to methamphetamine but no other illicit drugs and one containing children who met diagnosis criteria for ADHD but were not prenatally exposed to any illicit substance. Both groups of children completed intelligence measures to compute an IQ. Study results showed that the prenatally exposed children performed lower on the intelligence measures than their non-exposed peers with ADHD. The study results also suggest that prenatal exposure to methamphetamine may negatively impact processing speed as children develop.[38]
Alcohol[edit]
Maternal alcohol use leads to disruptions of the fetus’s brain development, interferes with the fetus’s cell development and organization, and affects the maturation of the central nervous system. Even small amounts of alcohol use can cause lower height, weight and head size at birth and higher aggressiveness and lower intelligence during childhood.[39] Fetal alcohol spectrum disorder is a developmental disorder that is a consequence of heavy alcohol intake by the mother during pregnancy. Children with FASD have a variety of distinctive facial features, heart problems, and cognitive problems such as developmental disabilities, attention difficulties, and memory deficits.[39]
Tobacco use[edit]
Tobacco smoking during pregnancy exposes the fetus to nicotine, tar, and carbon monoxide. Nicotine results in less blood flow to the fetus because it constricts the blood vessels. Carbon monoxide reduces the oxygen flow to the fetus. The reduction of blood and oxygen flow may result in miscarriage, stillbirth, low birth weight, and premature births.[40] Exposure to secondhand smoke leads to higher risks of low birth weight and childhood cancer.[41]
Infections[edit]
If a mother is infected with a disease, the placenta cannot always filter out the pathogens. Viruses such as rubella, chicken pox, mumps, herpes, and human immunodeficiency virus (HIV) are associated with an increased risk of miscarriage, low birth weight, prematurity, physical malformations, and intellectual disabilities.[42] HIV can lead to acquired immune deficiency syndrome (AIDS). Untreated HIV carries a risk of between 10 and 20 per cent of being passed on to the fetus.[43] Bacterial or parasitic diseases may also be passed on to the fetus, and include chlamydia, syphilis, tuberculosis, malaria, and commonly toxoplasmosis.[44] Toxoplasmosis can be acquired through eating infected undercooked meat or contaminated food, and by drinking contaminated water.[45] The risk of fetal infection is lowest during early pregnancy, and highest during the third trimester. However, in early pregnancy the outcome is worse, and can be fatal.[45]
Maternal nutrition[edit]
Adequate nutrition is needed for a healthy fetus. Mothers who gain less than 20 pounds during pregnancy are at increased risk for having a preterm or low birth weight infant.[46] Iron and iodine are especially important during prenatal development. Mothers who are deficient in iron are at risk for having a preterm or low birth weight infant.[47] Iodine deficiencies increase the risk of miscarriage, stillbirth, and fetal brain abnormalities. Adequate prenatal care gives an improved result in the newborn.[48]
Low birth weight[edit]
Low birth weight increases an infants risk of long-term growth and cognitive and language deficits. It also results in a shortened gestational period and can lead to prenatal complications.
Stress[edit]
Stress during pregnancy can have an impact the development of the embryo. Reilly (2017) states that stress can come from many forms of life events such as community, family, financial issues, and natural causes. While a woman is pregnant, stress from outside sources can take a toll on the growth in the womb that may affect the child’s learning and relationships when born. For instance, they may have behavioral problems and might be antisocial. The stress that the mother experiences affects the fetus and the fetus’ growth which can include the fetus’ nervous system (Reilly, 2017). Stress can also lead to low birth weight. Even after avoiding other factors like alcohol, drugs, and being healthy, stress can have its impacts whether families know it or not. Many women who deal with maternal stress do not seek treatment.
Similar to stress, Reilly stated that in recent studies, researchers have found that pregnant women who show depressive symptoms are not as attached and bonded to their child while it is in the womb (2017).[49]
Environmental toxins[edit]
Exposure to environmental toxins in pregnancy lead to higher rates of miscarriage, sterility, and birth defects. Toxins include fetal exposure to lead, mercury, and ethanol or hazardous environments. Prenatal exposure to mercury may lead to physical deformation, difficulty in chewing and swallowing, and poor motoric coordination.[50] Exposure to high levels of lead prenatally is related to prematurity, low birth weight, brain damage, and a variety of physical defects.[50] Exposure to persistent air pollution from traffic and smog may lead to reduced infant head size, low birth weight, increased infant death rates, impaired lung and immune system development.[51]
See also[edit]
- Prenatal memory
- Prenatal and perinatal psychology
- Fetal pig
- Timeline of human prenatal development
- Transplacental carcinogenesis
References[edit]
- ^ patient.info » PatientPlus » Antepartum Haemorrhage Last Updated: 5 May 2009
- ^ The Royal Women’s Hospital > antepartum haemorrhage Archived 8 January 2010 at the Wayback Machine Retrieved on 13 Jan 2009
- ^ Definitions and Indicators in Family Planning. Maternal & Child Health and Reproductive Health. Archived 25 January 2012 at the Wayback Machine By European Regional Office, World Health Organization. Revised March 1999 & January 2001. In turn citing: WHO Geneva, WHA20.19, WHA43.27, Article 23
- ^ Singh, Meharban (2010). Care of the Newborn. p. 7. Edition 7. ISBN 9788170820536
- ^ Schacter, Daniel (2009). «11-Development». Psychology Second Edition. United States of America: Worth Publishers. ISBN 978-1-4292-3719-2.
- ^ Saladin, Kenneth (2011). Human anatomy (3rd ed.). McGraw-Hill. p. 85. ISBN 9780071222075.
- ^ Wilcox AJ, Baird DD, Weinberg CR (1999). «Time of implantation of the conceptus and loss of pregnancy». N. Engl. J. Med. 340 (23): 1796–9. doi:10.1056/NEJM199906103402304. PMID 10362823.
- ^ Moore L. Keith. (2008). Before We Are Born: Essentials of Embryology and Birth Defects. Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-3705-7.
- ^ a b Daftary, Shirish; Chakravarti, Sudip (2011). Manual of Obstetrics, 3rd Edition. Elsevier. pp. 1–16. ISBN 9788131225561.
- ^ «Fetal development: MedlinePlus Medical Encyclopedia». medlineplus.gov. Retrieved 7 April 2021.
- ^ Illes J, ed. (2008). Neuroethics : defining the issues in theory, practice, and policy (Repr. ed.). Oxford: Oxford University Press. p. 142. ISBN 978-0-19-856721-9. Archived from the original on 19 September 2015.
- ^
- Harley, Trevor A. (2021). The Science of Consciousness: Waking, Sleeping and Dreaming. Cambridge, United Kingdom: Cambridge University Press. p. 245. ISBN 978-1-107-12528-5. Retrieved 3 May 2022.
- Cleeremans, Axel; Wilken, Patrick; Bayne, Tim, eds. (2009). The Oxford Companion to Consciousness. New York, NY: Oxford University Press. p. 229. ISBN 978-0-19-856951-0. Retrieved 3 May 2022.
- Thompson, Evan; Moscovitch, Morris; Zelazo, Philip David, eds. (2007). The Cambridge Handbook of Consciousness. Cambridge, United Kingdom: Cambridge University Press. pp. 415–417. ISBN 9781139464062. Retrieved 3 May 2022.
- ^ Henrichs, J. (2010). Prenatal determinants of early behavioral and cognitive development: The generation R study. Rotteram: Erasmus Universiteit.
- ^ a b Stein, Z., Susser, M., Saenger, G., & Marolla, F. (1972). Nutrition and mental performance. Science, 178(62),708-713.
- ^ Barker, D. J., Winter, P. D., Osmond, C., Margetts, B., & Simmonds, S. J. (1989). Weight in infancy and death from ischaemic heart disease. Lancet, 2(8663), 577-580.
- ^ Brown, A.S.; Susser, E.S.; Hoek, H.W.; Neugebauer, R.; Lin, S.P.; Gorman, J.M. (1996). «Schizophrenia and affective disorders after prenatal famine». Biological Psychiatry. 39 (7): 551. doi:10.1016/0006-3223(96)84122-9. S2CID 54389015.
- ^ Neugebauer, R., Hoek, H. W., & Susser, E. (1999). Prenatal exposure to wartime famine and development of antisocial personality disorder in early adulthood. Jama, 282(5), 455-462.
- ^ Brown, A. S., van Os, J., Driessens, C., Hoek, H. W., & Susser, E. S. (2000). Further evidence of relation between prenatal famine and major affective disorder. American Journal of Psychiatry, 157(2), 190-195.
- ^ Eisenberg, R. B. (1976). Auditory Competence in Early Life: The Roots of Communicate Behavior Baltimore: University Park Press.
- ^ Gerhardt, K. J., Otto, R., Abrams, R. M., Colle, J. J., Burchfield, D. J., and Peters, A. J. M. (1992). Cochlear microphones recorded from fetal and newborn sheep. Am. J. Otolaryngol. 13, 226–233.
- ^ Lecaneut, J. P., and Granier-Deferre, C. (1993). «Speech stimuli in the fetal environment», in Developmental Neurocognition: Speech and Face Processing in the First Year of Life, eds B. De Boysson-Bardies, S. de Schonen, P. Jusczyk, P. MacNeilage, and J. Morton (Norwell, MA: Kluwer Academic Publishing), 237–248.
- ^ Kisilevsky, B. S., Hains, S. M. J., Lee, K., Xie, X., Ye, H. H., Zhang, K., and Wang, Z. (2003). Effects of experience on fetal voice recognition. Psychol. Sci. 14, 220–224.
- ^ DeCasper, A. J., and Fifer, W. P. (1980). Of human bonding: newborns prefer their mother’s voices. Science 208, 1174–1176.
- ^ DeCasper, A. J., and Spence, M. J. (1986). Prenatal maternal speech influences newborns’ perception of speech sounds. Infant Behav. Dev. 9, 133–150.
- ^ Moon, C., Cooper, R. P., and Fifer, W. P. (1993). Two-day-olds prefer their native language. Infant Behav. Dev. 16, 495–500.
- ^ May, Lillian; Byers-Heinlein, Krista; Gervain, Judit; Werker, Janet F. (2011). «Language and the Newborn Brain: Does Prenatal Language Experience Shape the Neonate Neural Response to Speech?». Frontiers in Psychology. 2: 222. doi:10.3389/fpsyg.2011.00222. PMC 3177294. PMID 21960980.
- ^ King, Suzanne; St-Hilaire, Annie; Heidkamp, David (2010). «Prenatal Factors in Schizophrenia». Current Directions in Psychological Science. 19 (4): 209–213. doi:10.1177/0963721410378360. S2CID 145368617.
- ^ Lawn JE, Cousens S, Zupan J (2005). «4 million neonatal deaths: when? Where? Why?». The Lancet. 365 (9462): 891–900. doi:10.1016/s0140-6736(05)71048-5. PMID 15752534. S2CID 20891663.
- ^ Centers for Disease Control (2018). «Pregnancy Complications». Centers for Disease Control.
- ^ «About Teenage Pregnancy». Centers for Disease Control. 2018. Archived from the original on 2018.
- ^ Wendell, A. D. (2013). «Overview and epidemiology of substance abuse in pregnancy». Clinical Obstetrics & Gynecology. 56 (1): 91–96. doi:10.1097/GRF.0b013e31827feeb9. PMID 23314721. S2CID 44402625.
- ^ Lerma Castaño, Piedad Rocio; Montealegre Suarez, Diana Paola; Mantilla Toloza, Sonia Carolina; Jaimes Guerrero, Carlos Alberto; Romaña Cabrera, Luisa Fernanda; Lozano Mañosca, Daiana Stefanny (2021). «Prenatal, perinatal and postnatal risk factors associated with fine motor function delay in pre-school children in Neiva, Colombia». Early Child Development and Care. 191 (16): 2600–2606. doi:10.1080/03004430.2020.1726903. S2CID 216219379.
- ^ a b Fonseca, B. M.; Correia-da-Silva, G.; Almada, M.; Costa, M. A.; Teixeira, N. A. (2013). «The Endocannabinoid System in the Postimplantation Period: A Role during Decidualization and Placentation». International Journal of Endocrinology. 2013: 510540. doi:10.1155/2013/510540. PMC 3818851. PMID 24228028.
- ^ Irner, Tina Birk (November 2012). «Substance exposure in utero and developmental consequences in adolescence: A systematic review». Child Neuropsychology. 18 (6): 521–549. doi:10.1080/09297049.2011.628309. PMID 22114955. S2CID 25014303.
- ^ Fergusson, David M.; Horwood, L. John; Northstone, Kate (2002). «Maternal use of cannabis and pregnancy outcome». BJOG: An International Journal of Obstetrics & Gynaecology. 109 (1): 21–27. doi:10.1111/j.1471-0528.2002.01020.x. ISSN 1471-0528. PMID 11843371. S2CID 22461729.
- ^ «The US Opioid Crisis: Addressing Maternal and Infant Health». Centers of Disease Control and Prevention. 29 May 2019.
- ^ Mayes, Linda C. (1992). «Prenatal Cocaine Exposure and Young Children’s Development». The Annals of the American Academy of Political and Social Science. 521: 11–27. doi:10.1177/0002716292521001002. JSTOR 1046540. S2CID 72963424.
- ^ Brinker, Michael J.; Cohen, Jodie G.; Sharrette, Johnathan A.; Hall, Trevor A. (2019). «Neurocognitive and neurodevelopmental impact of prenatal methamphetamine exposure: A comparison study of prenatally exposed children with nonexposed ADHD peers». Applied Neuropsychology: Child. 8 (2): 132–139. doi:10.1080/21622965.2017.1401479. PMID 29185821. S2CID 25747787.
- ^ a b Mattson, Sarah N.; Roesch, Scott C.; Fagerlund, Åse; Autti-Rämö, Ilona; Jones, Kenneth Lyons; May, Philip A.; Adnams, Colleen M.; Konovalova, Valentina; Riley, Edward P. (21 June 2010). «Toward a Neurobehavioral Profile of Fetal Alcohol Spectrum Disorders». Alcoholism: Clinical and Experimental Research. 34 (9): 1640–1650. doi:10.1111/j.1530-0277.2010.01250.x. ISSN 0145-6008. PMC 2946199. PMID 20569243.
- ^ Espy, Kimberly Andrews; Fang, Hua; Johnson, Craig; Stopp, Christian; Wiebe, Sandra A.; Respass, Jennifer (2011). «Prenatal tobacco exposure: Developmental outcomes in the neonatal period». Developmental Psychology. 47 (1): 153–169. doi:10.1037/a0020724. ISSN 1939-0599. PMC 3057676. PMID 21038943.
- ^ Rückinger, Simon; Beyerlein, Andreas; Jacobsen, Geir; von Kries, Rüdiger; Vik, Torstein (December 2010). «Growth in utero and body mass index at age 5years in children of smoking and non-smoking mothers». Early Human Development. 86 (12): 773–777. doi:10.1016/j.earlhumdev.2010.08.027. ISSN 0378-3782. PMID 20869819.
- ^ Waldorf, K. M. A. (2013). «Influence of infection during pregnancy on fetal development». Reproduction. 146 (5): 151–162. doi:10.1530/REP-13-0232. PMC 4060827. PMID 23884862.
- ^ «World health statistics». World Health Organization. 2014.
- ^ Diav-Citrin, O (2011). «Prenatal exposures associated with neurodevelopmental delay and disabilities». Developmental Disabilities Research Reviews. 17 (2): 71–84. doi:10.1002/ddrr.1102. PMID 23362027.
- ^ a b Bobić, B; Villena, I; Stillwaggon, E (September 2019). «Prevention and mitigation of congenital toxoplasmosis. Economic costs and benefits in diverse settings». Food and Waterborne Parasitology (Online). 16: e00058. doi:10.1016/j.fawpar.2019.e00058. PMC 7034037. PMID 32095628.
- ^ Ehrenberg, H (2003). «Low maternal weight, failure to thrive in pregnancy, and adverse pregnancy outcomes». American Journal of Obstetrics and Gynecology. 189 (6): 1726–1730. doi:10.1016/S0002-9378(03)00860-3. PMID 14710105.
- ^ «Micronutrient deficiencies». World Health Organization. 2002. Archived from the original on 5 December 1998.
- ^ «What is prenatal care and why is it important?». www.nichd.nih.gov.
- ^ Reilly, Nicole (2017). «Stress, depression and anxiety during pregnancy: How does it impact on children and how can we intervene early?». International Journal of Birth & Parent Education. 5 (1): 9–12.
- ^ a b Caserta, D (2013). «Heavy metals and placental fetal-maternal barrier: A mini review on the major concerns». European Review for Medical and Pharmacological Sciences. 17 (16): 2198–2206. PMID 23893187.
- ^ Proietti, E (2013). «Air pollution during pregnancy and neonatal outcome: A review». Journal of Aerosol Medicine and Pulmonary Drug Delivery. 26 (1): 9–23. doi:10.1089/jamp.2011.0932. PMID 22856675.
Further reading[edit]
- MedlinePlus Encyclopedia: Fetal development
- Moore, Keith L. (1998). The Developing Human (3rd ed.). Philadelphia PA: W.B. Saunders Company. ISBN 9780721669748.
- Wilcox AJ, Baird DD, Weinberg CR (June 1999). «Time of implantation of the conceptus and loss of pregnancy». N. Engl. J. Med. 340 (23): 1796–9. doi:10.1056/NEJM199906103402304. PMID 10362823.
- Ljunger E, Cnattingius S, Lundin C, Annerén G (November 2005). «Chromosomal anomalies in first-trimester miscarriages». Acta Obstet Gynecol Scand. 84 (11): 1103–7. doi:10.1111/j.0001-6349.2005.00882.x. PMID 16232180. S2CID 40039636.
- Newman, Barbara; Newman, Philip (10 March 2008). «The Period of Pregnancy and Prenatal Development». Development Through Life: A Psychosocial Approach. Cengage Learning. ISBN 978-0-495-55341-0.
- «Prenatal Development – Prenatal Environmental Influences – Mother, Birth, Fetus, and Pregnancy.» Social Issues Reference. Version Child Development Vol. 6. N.p., n.d. Web. 19 Nov. 2012.
- Niedziocha, Laura. «The Effects of Drugs And Alcohol on Fetal Development | LIVESTRONG.COM.» LIVESTRONG.COM – Lose Weight & Get Fit with Diet, Nutrition & Fitness Tools | LIVESTRONG.COM. N.p., 4 Sept. 2011. Web. 19 Nov. 2012. <http://www.livestrong.com/article/535499-the-effects-of-drugs-and-alcohol-on-fetal-development/>.
- Jaakkola, JJ; Gissler, M (January 2004). «Maternal smoking in pregnancy, fetal development, and childhood asthma». American Journal of Public Health. 94 (1): 136–40. doi:10.2105/ajph.94.1.136. PMC 1449839. PMID 14713711.
- Gutbrod, T (1 May 2000). «Effects of gestation and birth weight on the growth and development of very low birthweight small for gestational age infants: a matched group comparison». Archives of Disease in Childhood: Fetal and Neonatal Edition. 82 (3): 208F–214. doi:10.1136/fn.82.3.F208. PMC 1721075. PMID 10794788.
- Brady, Joanne P., Marc Posner, and Cynthia Lang. «Risk and Reality: The Implications of Prenatal Exposure to Alcohol and Other Drugs .» ASPE. N.p., n.d. Web. 19 Nov. 2012. <http://aspe.hhs.gov/hsp/cyp/drugkids.htm>.
External links[edit]
Wikimedia Commons has media related to Embryology.
- Chart of human fetal development, U.S. National Library of Medicine (NLM)
- U.K. Human Fertilisation and Embryology Authority (HFEA), regulatory agency overseeing the use of gametes and embryos in fertility treatment and research